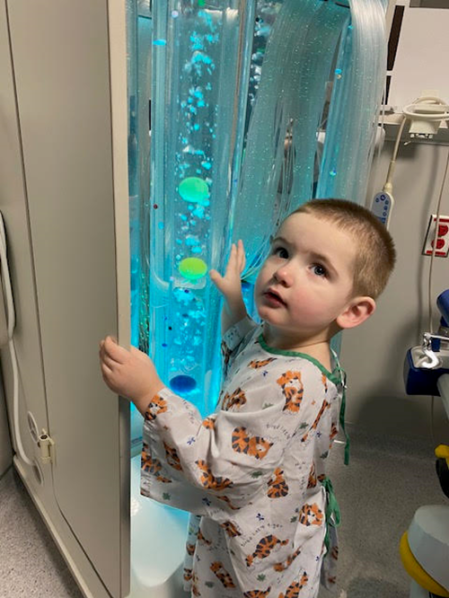
At first glance, two-year-old Jedi Ruzicka is not only unassuming but, also frankly, adorable. Jedi has plump cheeks and a dimple on his chin. His ears protrude slightly, giving him an almost cartoonish appearance. Like other children his age, Jedi is rowdy. He enjoys trips to the beach and the waterpark, and sledding.
However, Jedi wasn’t always full of energy—in fact, prior to medical intervention, he was “zombie-like,” according to his parents. He is currently unable to speak in full sentences and struggles with learning disabilities, which have worsened since he consumed lead-based paint six months ago. Jedi’s case is symptomatic of the widespread exposure to lead faced by many Chicago-area children.
It may come as a surprise to parents that lead poisoning is far from unusual in the city. In 2021, there were approximately 1,100 unique cases of children with an elevated blood lead level of over 5 micrograms per deciliter (μg/dl), according to data from the Chicago Department of Public Health (CDPH).
Jedi is just one of the thousands of children who come into contact with lead each year.
“After the diagnosis, I kind of immediately knew. It was like, oh, he got it from the bedroom window,” said Alainah Long, Jedi’s mother.
She believes that her son swallowed paint flakes at their apartment in the Northwest Chicago neighborhood of Belmont Cragin, where they lived for just under a year.
According to the Centers for Disease Control and Prevention (CDC), lead exposure can have adverse effects on children, including brain and nervous system damage, slowed growth, and problems with learning, behavior, and speech. Furthermore, there is evidence that this exposure can cause long-term harm.
Long and her husband, Joseph Ruzicka, did not suspect that their son was in danger when they moved in. The apartment was updated and spacious enough to accommodate the pair and their five children. The kitchen was freshly remodeled, sporting granite countertops and new cabinets. The building was situated on a quiet street lined with trees.
However, unbeknownst to the couple, lead paint covered the windowsills and walls throughout the building.
“Jedi learned to crawl at that apartment,” Ruzicka said. He believes that Jedi came into contact with lead dust on the floor, then put his hands in his mouth. He suspects the toddler ate paint chips, too, as Jedi had a history of compulsively consuming non-food items.
The family of seven had occupied the space for just under a year when Long and Ruzicka noticed that their son was falling behind developmentally. He was failing to do things that were expected at his age, like starting to talk and making eye contact. He struggled to pay attention and continued to eat non-food items.
Ultimately, after their son’s condition failed to improve, Jedi’s parents decided to voice their concerns to his pediatrician.
“He kind of just seemed like he was in his own world for the most part,” Long said. “So we started talking to his pediatrician and she ended up doing a blood test and then it came back with lead poisoning and it kinda all came together.”[1]
During a routine visit to Rush University Medical Center last October, Long told the doctor that she was concerned about Jedi’s cognitive delays and eating habits. Jedi was just over a year old at the time.
The doctor referred him for audiology and neurology screening, as well as special education, a range of services designed to help kids with learning disabilities. The doctor also performed bloodwork.
While this newfound responsibility was enough to deal with on its own, Jedi’s parents were about to receive even more shocking news.
The following day, the first round of blood test results returned, showing that Jedi was anemic. A day later, more results showed that he had a blood lead level of 76.4 micrograms per deciliter (μg/dL). (For reference, the Centers for Disease Control and Prevention use 3.5 μg/dL as a benchmark for children with elevated blood lead levels.)
Long and Ruzicka took Jedi to the emergency room at Rush. He was subsequently transferred to the intensive care unit at Comer Children’s Hospital at the University of Chicago.
Anita Raghavan, Clinical Associate of Pediatrics at Comer Children’s Hospital, is familiar with Jedi’s case. While she did not treat Jedi herself, she is a member of the team that did, and spoke as a representative.
“His lead level was extremely high because it was over the level of 44 (μg/dL),” Raghavan said. “45 (μg/dL) and above generally necessitates admission to the hospital for treatment of lead toxicity.”
If a patient’s blood lead level registers over 45 micrograms, the CDC recommends that healthcare providers consider admitting the child to the hospital if the patient’s home is not lead-safe, if they are unable to find a lead-free living space, or if the source of lead exposure has yet to be identified. If the patient exhibits potentially life-threatening symptoms such as seizures, coma, or vomiting, the CDC recommends admission to the hospital as soon as possible.
Despite instating blood lead level benchmarks, the CDC insists that there is no safe lead level .“There are certain pockets and communities where lead poisoning is more prominent,” Raghavan
said. “All children below the age of three get screened. And then higher risk kids between the ages of three and six continue to get screened. So it’s a large population for us that we’re screening.”
In an email, a spokesperson from the CDPH wrote, “We’ve made tremendous progress since the late 1990s, when 25% of Chicago children had elevated blood lead levels (≥10 ug/dL). Today, less than one percent of Chicago children reach that level. Between 2017 and 2021 alone, we’ve decreased from about 2.4% of children having a blood lead level of five or higher so at that lower level to 1.8%.”
However,the spokesperson conceded that all zip code areas in Chicago are considered high-risk for lead.
The CDPH recommends that all children in Chicago should be tested for lead by the child’s regular medical provider during their routine well-child checks.
If Jedi hadn’t been tested at 18 months old, their parents wouldn’t have known about his lead poisoning. While children need proof of lead testing upon enrollment in daycare or kindergarten, there is no requirement for earlier testing. The CDPH recommends, but does not require, a blood lead level test for all children at 12, 24, and 36 months of age.
Jedi’s case is particularly difficult, as medical professionals are unable to determine how far the effects of lead exposure go. Upon his admission to Comer Children’s Hospital, doctors noted that Jedi appeared anemic. Lead prevents the body from absorbing iron efficiently and blocks the body’s ability to make new red blood cells, so patients exposed to lead toxicity often present with ion deficiency anemia. However, Jedi was a particularly enthusiastic milk drinker since birth, and milk also blocks the body’s ability to absorb iron.
Raghavan suspects that Jedi’s pica, or consumption of non-food items, was the result of anemia, as pica is often associated with iron deficiency. However, Raghavan is unable to draw any correlation between these symptoms and his later diagnosis of lead poisoning, though she acknowledges that a connection is possible.
“With lead toxicity, you can sort of present with some pica, so it’s hard to know which one came first. Additionally, we typically don’t make that diagnosis before the age of two because of the developmental reasons why kids put things in their mouth,” Raghavan said. “So it all circles back. It’s just this big, confusing circle.”
In the hospital, Jedi completed a course of medication to expel the lead from his body. Through this process, called chelation therapy, the medication bind with lead so it can be excreted in urine. The toddler was then given iron supplements, as his iron stores were empty.
In the following days, a health inspector from the CDPH visited the family’s rental apartment. An examination found traces of lead not only in their unit, but throughout the building, namely in the hallways and back and front porches. Representatives from the CDPH told the family that the paint in the apartment dated back to the 1970s, only a few years before it was banned for residential use.
The inspector noticed a rubber mat stapled to the staircase. He said that it was a standard solution from the CDPH and speculated that an inspector had already been at the building. However, he could not locate any records of such a visit.
Regardless, the inspector taped a form to the front door following his visit. It reads, in part, “Other units in the building may not have been tested. Units not tested may also have lead hazards.” The letter emphasizes that the CDPH requires all children 6 months to 6 years of age to undergo an annual blood lead test. It instructs parents to ask their child’s doctor to order a lead test if they haven’t been tested recently, and lists number to call for more information.
A building owner has six months to come into compliance following inspection, according to the CDPH spokesperson. If lead abatement has not taken place in a timely manner, the case will be referred to court, which will determine any fines against the building owner. In 2022, the CDPH referred 32 homeowners to court.
However, the spokesperson declined to comment on Jedi’s case.
Under federal law, landlords are required to disclose knowledge of the presence of lead-based paint to each tenant planning to lease any portion of a residential dwelling built before 1978.
Ruzicka tells me that the landlord, Edgar Espinosa, did none of this.
Espinosa denied knowing about the lead in a recent interview with CBS News Chicago. CBS 2 viewed the family’s lease and noted that the lease is missing check marks next to the “lead notification requirement,” in line with Ruzicka’s claims.
The family has not returned to the apartment since then.
“Nothing’s been fixed there, as far as we know,” Ruzicka said. “And it’s just sad because other children do live there. It’s sad to know the city won’t go into those apartments and inspect until their child has lead poisoning.”
The family stayed in a hotel for 10 days, as Jedi was unable to leave the hospital unless they found somewhere else to live.Out of options, the couple emptied their savings into a new apartment in the same neighborhood, wanting to keep the children in the same school district and maintain some semblance of normalcy in their lives.
As it stands, Jedi’s diagnosis includes autism spectrum disorder and mixed receptive-expressive language disorder, meaning he struggles to communicate and to understand others’ words.
While it is unclear if Jedi’s learning disabilities were directly caused by lead poisoning, the toddler still has over 10 micrograms of lead in his blood. Fortunately, his levels dropped to 14.9 μg/dL at the most recent reading.
Jedi’s medical records show that he is receiving an array of treatments to tackle issues. Following release from the hospital, he began with outpatient speech and occupational therapy. The toddler completed eight out of 12 sessions, stopping only because Early Invention started and was taking place at home, which was a lot more convenient for the family. Early Intervention is a state-sponsored program for children with developmental delays and learning disabilities.
Jedi’s therapy sessions have increased in frequency. He now attends each one twice per week. He also receives feeding and developmental therapy, and his parents recently found a healthcare provider for physical therapy, which will begin this month.
However, all this requires a lot of coordination on his family’s part.
“It’s been rough all around,” Long said. “Before, I didn’t have a set schedule. Now I have one of those daily journal things and I’m like, lemme see what I gotta do today. What’s tomorrow? When is this appointment? When’s that appointment?”
“And now I can’t make plans for a certain day ’cause we have to do therapy or you know, everything’s revolving around Jedi. Which I have no problem with it being,” she said. “For Early Intervention, we had a meeting to see how things were going and they were like, ‘I know this is a lot on you.’”
Yet, Long finds reasons to be optimistic. Jedi is learning basic sign language instead of proper speech, and while he has a ways to go, he is improving. Recently, after finishing a bowl of macaroni, Jedi rotated his palms to signal “all done.”
“And I wanted to cry so bad because he was, like, speaking to me, but in silence,” Long said.

Jedi’s diet has also grown more complex. According to Long, his former diet was restricted to three or four actual food items. Now he likes steak, sausage and bacon. He likes soft pretzels. He likes eggs, rice and Jello. And chicken nuggets. He still loves milk, but his parents are trying to wean him off it by giving him glasses of water when he wakes in the middle of the night.
And while Jedi has “a lot more personality now,” there are trade-offs.
“We do see the bad side of it,” Long said. “His aggression. He likes throwing things and hitting people with stuff, so he is constantly hitting his brother and his sister over the head with Nerf guns and stuff. They’re good with it, but he just needs a little extra love compared to everybody.”
Aggression is a well-documented effect of lead poisoning in children, with ripple effects lasting into adulthood. The National Institutes of Health cited studies showing that exposure causes “externalizing behavior problems,” including aggressiveness and bullying.
According to a fact sheet from Loyola University Chicago, lead poisoning can be linked to childhood delinquency, and has even been connected to more arrests, including those for violent offenses, in adults.
Despite the challenges, both current and anticipated, Jedi’s family remains supportive. Jedi’s older siblings, aged nine and 11, are “real helpful with him, even though he doesn’t really like being by them so much,” Long said.
Jedi has his loving side, too. He’ll feed his nine-month-old sister her bottle. He enjoys playing with three-year-old Giovanni, whom Long refers to as “his twin.” (The duo wear matching clothing.)
“He is really loving and wants that connection with someone,” Long said of Jedi. “I think that’s one of his best traits.”
Of herself, she said, “As a mom, I can’t give up on my kids. So I have to make it happen. No matter what it is, whatever it takes, I gotta do it. That’s how I look at things.”
This level of dedication is evidenced by her appearance, as Long’s body is etched with tattoos bearing the names of her children. Giovanni’s name, for instance, is written in ornate cursive across her forearm. Jedi’s name is stamped on her left fist. She and her husband have matching tattoos on that spot.
“It’s been like a mix of emotions, this whole thing,” Long says. “Seeing him progress as the levels go down, it makes me happy. At the same time, it makes me sad because he should have been doing these things, you know, but like, I’m happy he’s doing them now.”
The couple expressed their desire for other families to know about Jedi’s story, to prevent similar things from happening to them.

“If parents have suspicions or their child’s having delays, they should bring that up to their pediatrician because a lot of times they’ll want to wait for them to grow out of it. I don’t think that’s something to wait to do,” Long said.
At a local level, the CDPH provides support for children suffering from lead toxicity.Whenever a child’s blood test indicates an elevated level of lead, the organization assigns a nurse case manager to the family. The nurse will visit the home, complete a social developmental assessment, provide nutritional counseling and make referrals for additional services the family may need.
The CDC also suggests a five-step process to lower a child’s blood lead level, beginning with talking to the child’s doctor to determine the best treatment. It is crucial to find the source of lead in the home and to clean it up as best as possible. The agency provides dietary suggestions for calcium-rich foods like yogurt, cheese and spinach; iron-rich foods like beans, peanut butter and lean red meat; and foods containing vitamin C like oranges and peppers.
Of course, the best way to avoid complications of lead toxicity is to prevent lead exposure in the first place. The CDC provides guidelines in this area as well. Parents can make their home lead-safe by checking common sources of lead like paint, drinking water, and products like children’s toys, antique or imported kitchenware, and traditional medicines and cosmetics.
Long and Ruzicka are fortunate for the ongoing support of doctors and care providers involved with Jedi’s case. The family also has a GoFundMe to help with medical expenses.
Amid the ever-evolving circumstances, Jedi’s parents remain optimistic.
“With the therapies, we’re just hoping for a good outcome,” Long said. “I don’t know how long it’s gonna take. We don’t know. So we’re just hoping, one day at a time.”


